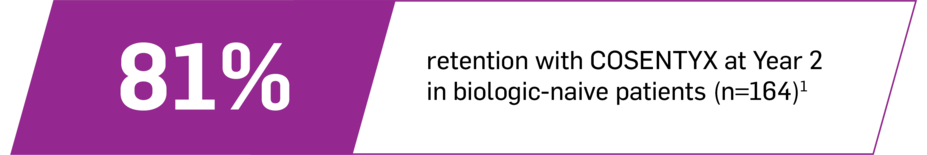
COSENTYX works as early as 3 weeks with results out to 2 years1
2x improvement vs placebo: 40% of biologic-naive patients achieved ASAS40 at 1 year on COSENTYX 150 mg no load (n=166) vs 20% on placebo (n=171) (NRI, P<0.05) (PREVENT* primary end point)5
ASAS40 responses at Week 3 in biologic-naive patients: 24% for COSENTYX 150 mg (n=164) and 15% for placebo (n=171)2
In PREVENT, ASAS40 was a prespecified exploratory end point at Week 3. No clinical or statistical conclusions can be drawn.2
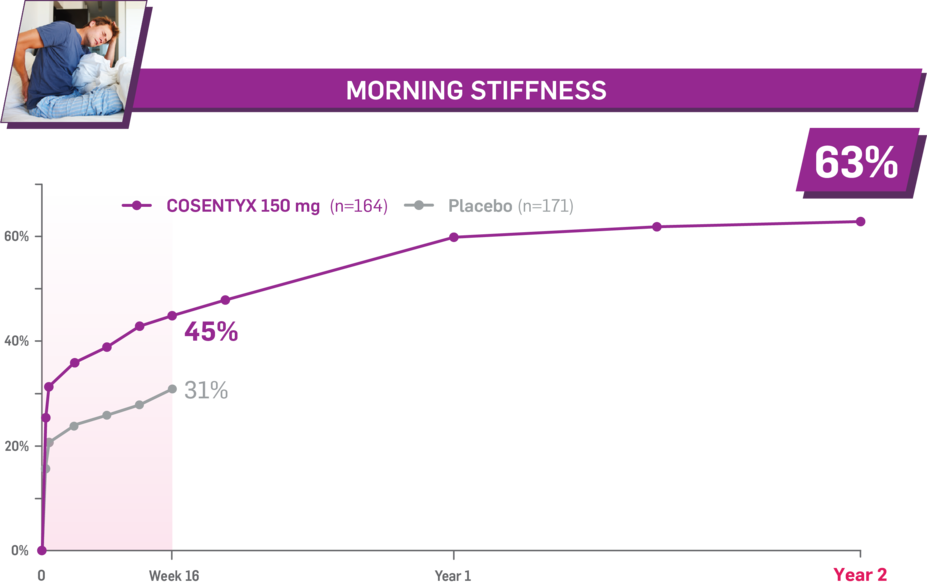
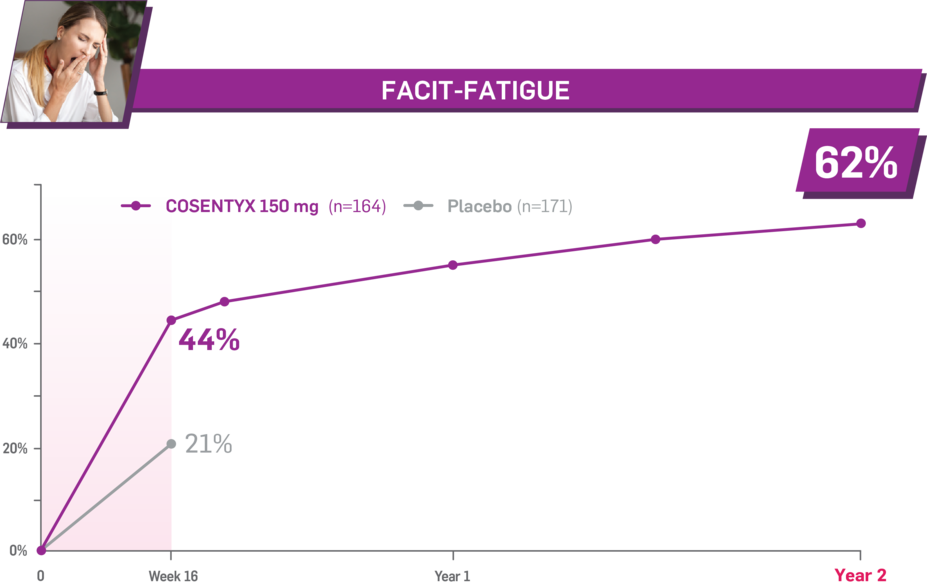
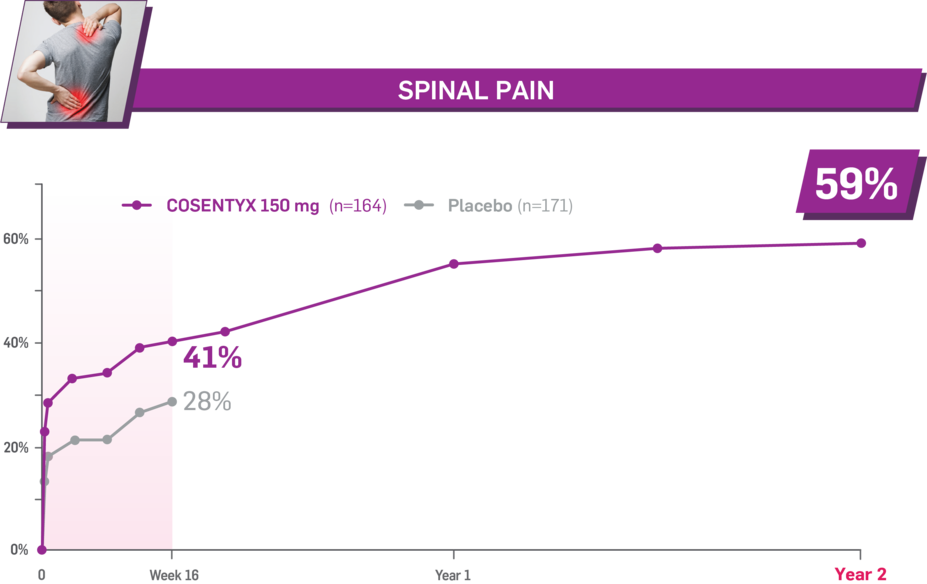
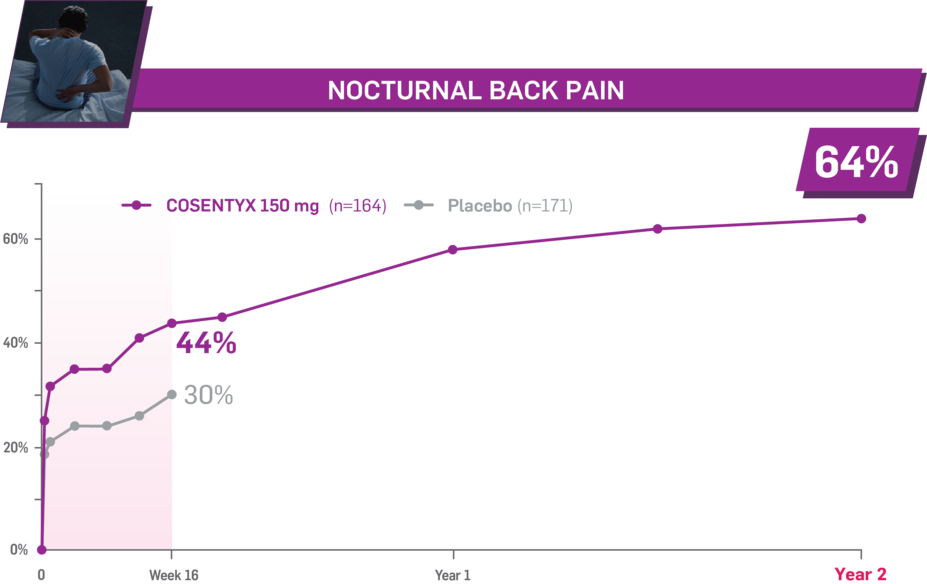
Durable improvement in mean scores in biologic-naive patients with nr-axSpA (PREVENT; mean % for COSENTYX 150 mg)1
In PREVENT, the below measures were prespecified exploratory end points in subgroups of biologic-naive patients through Year 2. No clinical or statistical conclusions can be drawn.2
Mean baseline morning stiffness score at Week 16: 7.2 and 6.6 (150-mg load and placebo groups, respectively); at Year 2: 7.2 (150-mg load group). Morning stiffness was measured by the mean of the 2 BASDAI scores from questions 5 (duration) and 6 (severity), measured on a 0 to 10 numeric response scale.1,2
Mean baseline fatigue score at Week 16: 21.8 and 24.0 (150-mg load and placebo groups, respectively); at Year 2: 21.9 (150-mg load group). Fatigue was measured by FACIT-Fatigue, a 13-item questionnaire that assesses self-reported fatigue and its impact on daily activities and function.1,2
Mean baseline spinal pain score at Week 16: 73.5 and 71.1 (150-mg load and placebo groups, respectively); at Year 2: 73.5 (150-mg load group). Spinal pain was measured using a 100-mm VAS as a component of ASAS.1,2
Mean baseline nocturnal back pain score at Week 16: 70.8 and 70.8 (150-mg load and placebo groups, respectively); at Year 2: 70.9 (150-mg load group). Nocturnal pain was measured using a 100-mm VAS as a component of ASAS.1.2
*Trial used SC administration.
†The effectiveness and safety of COSENTYX IV formulation are based on the pharmacokinetic exposure and extrapolation of the established effectiveness and safety of SC COSENTYX in adult patients with active PsA, AS, or nr-axSpA.4
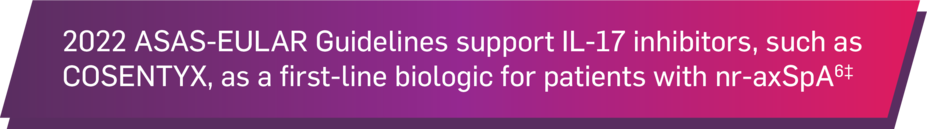
‡The updated ASAS-EULAR 2022 Guidelines are based on 2 systematic literature reviews of nonpharmacologic and nonbiological pharmacologic treatment and bDMARDs for nr-axSpA and AS. The recommendations were developed by a steering committee and task force of members from Europe and North America. Novartis is one of the many corporate supporters of the ASAS-EULAR network.6
Definitions
AS, ankylosing spondylitis; ASAS, Assessment of SpondyloArthritis International Society criteria; axSpA, axial spondyloarthritis; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; bDMARDs, biologic disease-modifying antirheumatic drugs; EULAR, European Alliance of Associations for Rheumatology; FACIT, Functional Assessment of Chronic Illness Therapy; IL, interleukin; IV, intravenous; nr-axSpA, non-radiographic axial spondyloarthritis; PsA, psoriatic arthritis; SC, subcutaneous; VAS, visual analog scale.
References
1. Data on file. CAIN457H2315 (PREVENT): Data Analysis Report. Novartis Pharmaceuticals Corp; August 2021.
2. Data on file. CAIN457H2315 (PREVENT): Clinical Study Report. Novartis Pharmaceuticals Corp; November 2019.
3. Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777-783.
4. Cosentyx. Prescribing information. Novartis Pharmaceuticals Corp.
5. Deodhar A, Blanco R, Dokoupilová E, et al. Improvement of signs and symptoms of nonradiographic axial spondyloarthritis in patients treated with secukinumab: primary results of a randomized, placebo-controlled phase III study. Arthritis Rheumatol. 2021;73(1):110-120 and Supplementary Material.
6. Ramiro S, Nikiphorou E, Sepriano A, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis. 2023;82(1):19-34.